A lower dose of conventional 3D conformal radiotherapy worked just as quicky in cancer patients with solid organ tumours.
Patients with less than a month to live should not be subjected to dose-escalated stereotactic body radiotherapy for painful bone metastases, according to new research.
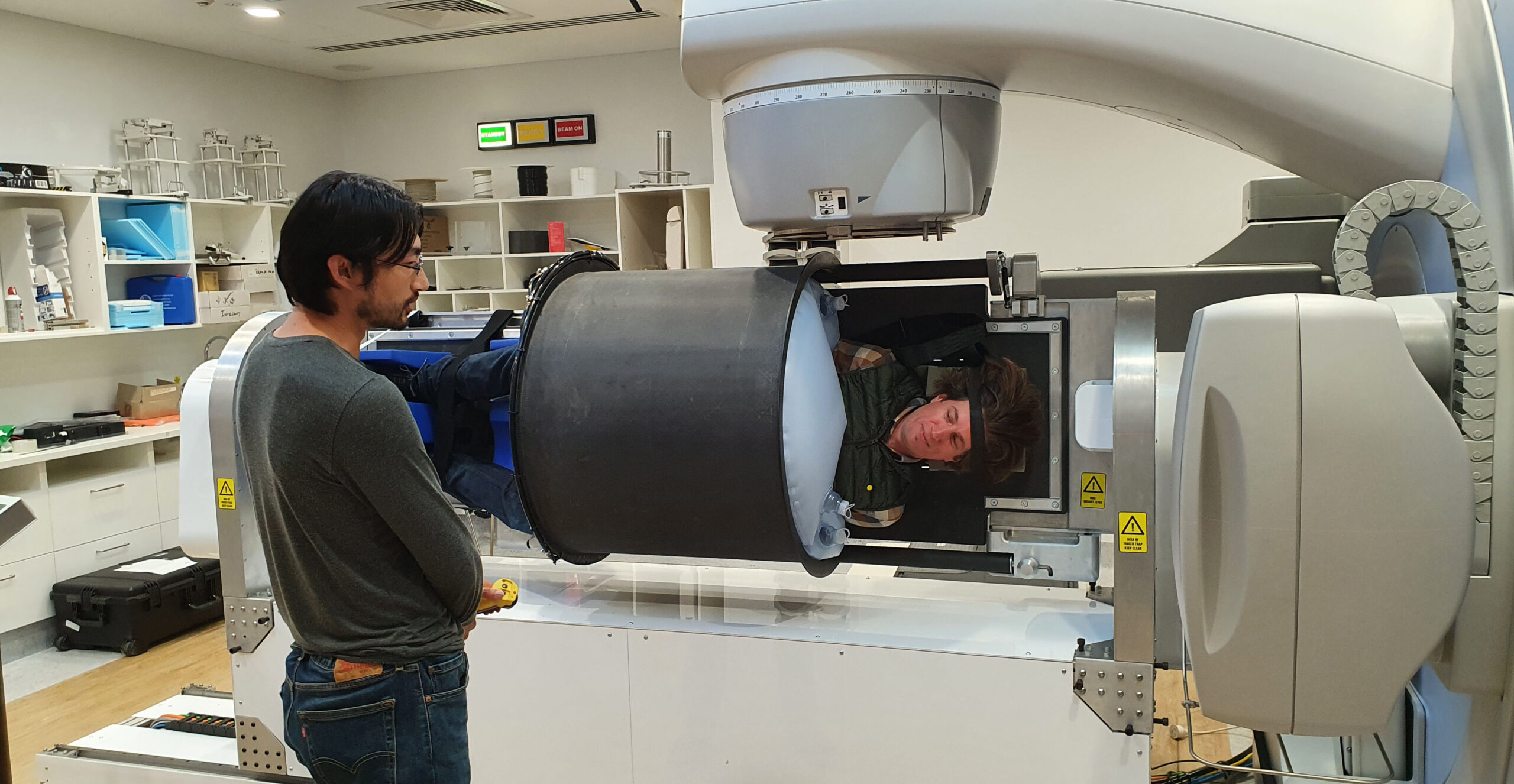
Solid cancers commonly lead to painful bone metastases, and radiation therapy – typically three-dimensional conformal radiotherapy – is often used to address the pain and other symptoms. Ablative stereotactic body radiotherapy (SBRT) can also be used, although the safety and efficacy of this approach is unclear.
Now, new Belgian research suggests that SBRT fails to reduce self-reported pain four weeks after treatment compared to 3D-CRT, suggesting the newer approach is not beneficial for patients with a shorter predicted survival.
One hundred and twenty-six patients with painful bone metastases arising from a solid primary tumour received either 3D-CRT or SBRT as part of the multicentre phase 3 trial, and were followed up at one, three, six, nine and 12 months after treatment. The majority of patients had either lung (32%), prostate (24%) or breast (16%) cancer.
At the one-month follow-up there was no difference in the primary outcome – the proportion of patients with a complete response to the radiotherapy (i.e., a pain score of 0 and no increase in analgesic use) – between the two groups (25% for the 3D-CRT arm and 37% in the SBRT arm). The results at the three-month follow-up were similar; 24% for the 3D-CRT group and 33% for the SBRT group.
Related
The researchers were not surprised by the findings.
“The initial idea that dose-escalated SBRT induces faster and earlier pain relief, as commonly assumed when this trial was designed, is currently no longer considered valid,” they wrote in the Journal of Clinical Oncology.
“However, the durability of the response is far more of an issue now, particularly as patients with metastatic cancer have continuously improving survival rates.”
Other outcomes, such as the proportion of patients experiencing a pain flare (27% versus 18%), receiving prophylactic or symptomatic corticoids (3% each) or grade 2-3 toxicity (14% versus 15%) were also similar between groups. In addition, there was no difference or changes in patient-reported quality of life.
“Our results indicate that dose-escalated SBRT for patients with survival of a month or less is not beneficial,” the researchers concluded.
“There is arguably a subset of patients with a survival of at least [three] months who do benefit, but further selection is crucial.”