Mechanical stress in tiny blood vessels appears to reprogram tumour cells into a more aggressive state, offering new clues to how metastasis begins.
The physical stress of travelling through the body’s tiniest blood vessels may trigger tumour cells to become more aggressive, according to new UNSW research.
Nine of the 10 most common cancer deaths in Australia are due to solid tumours, and in most cases it is not the primary growth, but the spread to distant organs, that proves fatal.
The process of metastasis has long puzzled oncologists: why do only a small fraction of circulating tumour cells survive the bloodstream and colonise distant tissues, yet rates of metastasis remain high in certain cancers?
A new study published in Nature Communications points to a surprising answer.
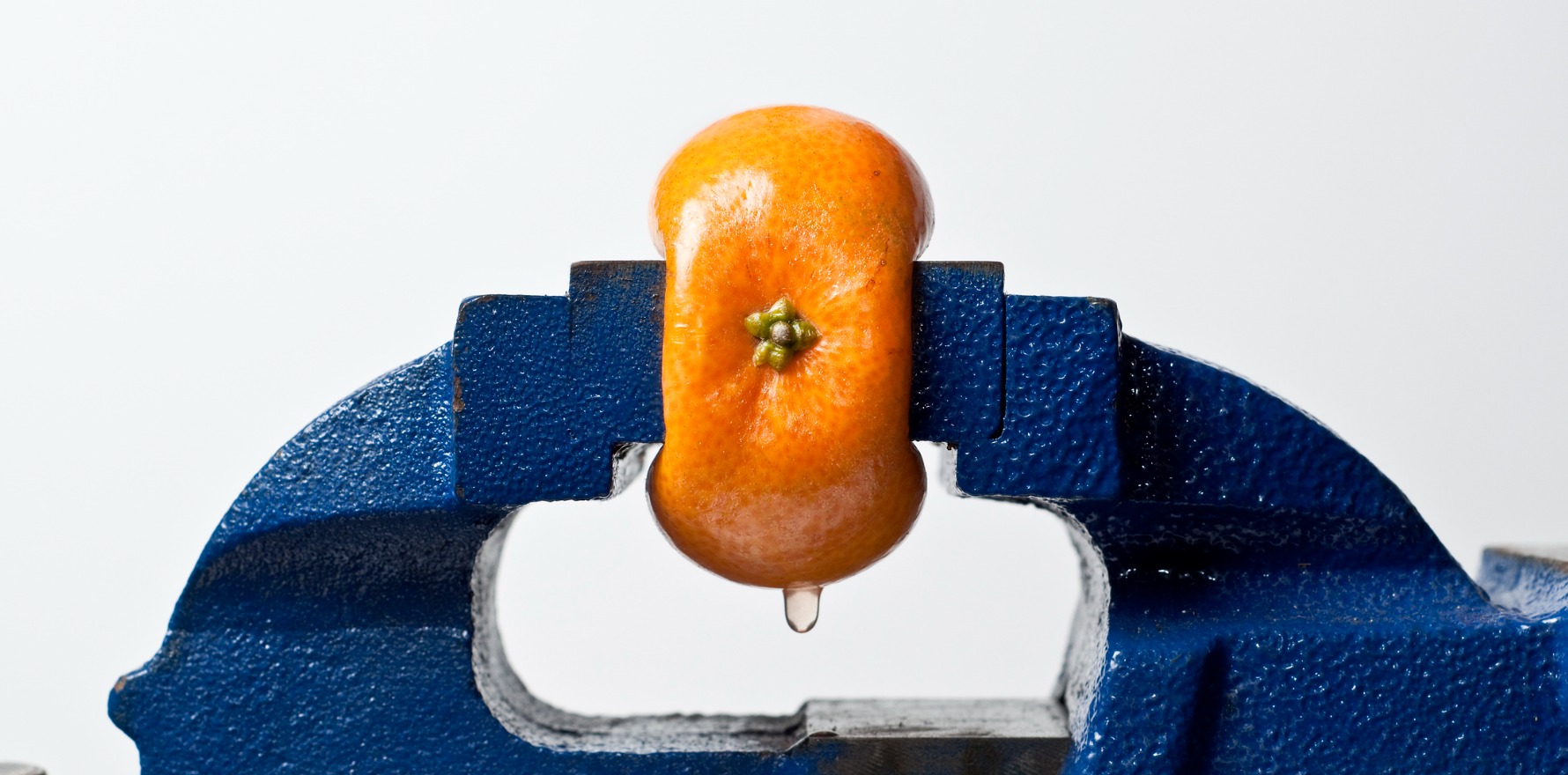
Researchers have discovered that the mechanical squeezing of cancer cells as they pass through the body’s narrowest blood vessels may itself trigger them to change state, becoming more aggressive and tumour-forming.
When forced through channels smaller than 10 micrometres – about a fifth the width of a human hair – melanoma cells began to resemble stem cells, with traits that enhance survival, plasticity and the ability to seed new tumours.
The finding supports a theory long held by medical researchers that the mechanical pressure of narrow blood vessels might make cancer cells more aggressive.
While the recent results were observed in bioengineered devices in the lab and in mice, they offer a new perspective that could inform further research and future strategies to prevent cancer from spreading, said co-author UNSW Professor Kris Kilian.
“For a long time we’ve not fully understood how cancer spreads to distant organs,” he said.
“Most tumour cells circulating in blood are ill equipped to survive and spread to other organs, but we still see high rates of metastasis in some patients.
“Our finding paints a new picture, where cancer cells are triggered into becoming more tumorigenic – meaning they can form new tumours – after squeezing through the narrowest of spaces, suggesting this process may precede events like bone and brain metastasis.”
As part of the study, the researchers designed a specialised “microfluidic” device, smaller than a postage stamp, that replicated the way blood flows through progressively narrower vessels.
Lead author Dr Giulia Silvani, working at the Australian National Fabrication Facility, created the channels from PDMS, a biocompatible rubbery plastic, ranging from 30 micrometres down to just five.
She then pumped a nutrient solution containing human melanoma cells through the channels at the flow rates seen in living capillaries.
Within 15 minutes, the cells that emerged from the smallest passages were visibly deformed. Molecular analysis showed that these cells expressed proteins associated with stemness, survival and metastatic potential.
The team then asked whether these mechanically stressed cells behaved differently in vivo.
Injecting the “squeezed” melanoma cells into immunodeficient mice, they observed that the animals developed significantly more tumours in the lungs, bones and brain after 30 days compared with mice given unsqueezed cells.
The results strongly suggest that the act of being forced through tiny blood vessels can reprogram cancer cells into a more aggressive state.
“One of the most exciting aspects of this project was the chance to study metastatic cancer cells in a way that hasn’t been possible before,” said Dr Silvani.
“Their journey through the body is so hidden, leaving little trace and making them incredibly difficult to capture in action. But we were able to recreate that journey in the lab, giving us a rare glimpse into the moment when these cells switch into their most aggressive state.
“Being able to uncover even a small part of that mystery feels like an important step towards understanding, and ultimately stopping, the spread of cancer.”
The implications for clinical oncology are considerable. If capillary transit can drive metastasis, then patients’ risk profiles may depend not only on their tumour’s biology but also on the vascular environments those tumours encounter.
“These results open up new possibilities for prognosis and treatment, by targeting the mechanical forces that lead to metastasis,” said Professor Kilian.
“We could then look at the cancer cells found in a patient’s blood stream to study their susceptibility to this sort of transformation which could help us assess the risk of metastasis for that individual.
“Or we could use MRI or other imaging techniques to identify regions with high densities of micro vessels to monitor for metastasis, possibly even intervening to make it much harder for the cells to get to these small capillaries.
“The point is, it used to be thought that it was just this extremely rare type of cell that found its way from a primary tumour to a spot where they could invade. But no, in some cases it’s actually the squeezing that changes the cell into this rare type, and it could put cancer researchers in a much stronger position to devise new treatment strategies.”
About 90% of the work for this project focussed on melanoma cancer cells, but Professor Kilian said he was hopeful the same conclusions will be drawn when researchers look at the squeezing effect on free-floating cells from other cancer tumours.
“I believe we’ll find evidence that many solid tumours metastasise this way – for instance, we’re already seeing compelling evidence when we repeat these experiments with breast cancer – and I’m looking forward to testing a range of cancer cell types in the lab,” he said.
“But I’m glad we began our study with melanoma cells, since skin cancer has such high mortality rates in Australia when it spreads to other organs. It’s vitally important that we gain a better understanding of melanoma metastasis, to better treat those suffering from this deadly disease.”
For Dr Silvani, the work also illustrated the power of combining engineering and biology.
“Watching this idea grow from a spark of intuition into a real discovery has been deeply inspiring,” she said.
“It’s a powerful reminder of what can be achieved when engineering and biology come together. Cells are intricate machines, and unravelling their mysteries requires precise design and innovative tools, guided by the insights biology provides.”