Minimally invasive treatments are a viable alternative for some kidney cancer patients
The incidence of renal cell carcinoma (RCC) is increasing within Australia, reflecting a global uptick in kidney cancers.1 Around 4,600 Australians were diagnosed with kidney cancer in 2023, with a median age of 65, with RCC accounting for about 90% of all cases.2
The traditional treatment landscape for RCC has been dominated by major surgery, specifically radical or partial nephrectomy.3 However, along with the increasing incidence, the mean age at which RCC is diagnosed is also increasing.4 As the Australian population ages, the demand for alternative treatments that minimise risks and recovery time in this population, whilst maintaining effectiveness will only continue to grow. Ablation, specifically cryoablation, for RCC is the only non-surgical treatment modality with long term data that fills this need.5
Although surgery is the benchmark for long-term treatment, it is a riskier proposition in the elderly and comorbid. Complications of surgical intervention can include bleeding and infection, long-term impacts on kidney function, prolonged hospital stays and post-operative care, which can result in considerable impact on the patient and strain on the healthcare system. Shorter recovery periods, preservation of renal function and lower post-operative pain are advantages of cryoablation, with respect to surgery.7 Furthermore, meta-analyses suggest that cancer-related outcomes are equivalent between the modalities.1,6,7 This, multiple oncological, urological and interventional radiological guidelines suggest ablative therapies as part of the treatment armamentarium for small renal masses.4,8-10
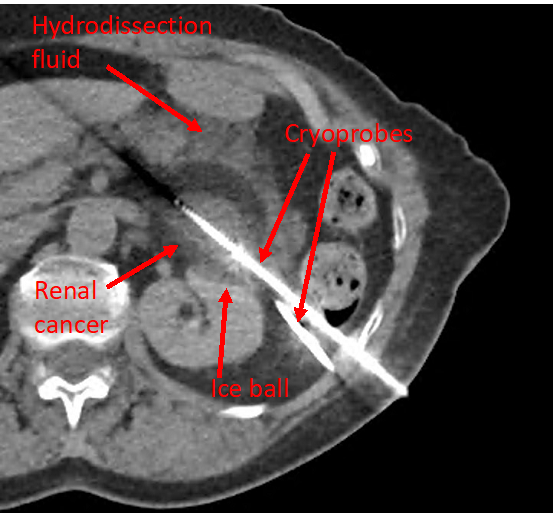
Performed by an interventional radiologist (IR), cryoablation for RCC is a procedure in which cryoprobes, usually between two and four, are inserted into the malignant mass via tiny incisions under imaging guidance. Further techniques, such as hydrodissection and pyeloperfusion, can be employed by the IR, if necessary. Once the needles are safely positioned, the freezing process is initiated. Ongoing computed tomography (CT) imaging throughout the procedure allows visualisation of the growing ice ball.
Cryoablation provides the ability to treat larger tumours and perform more technically challenging procedures when compared to older technology, such as radiofrequency (RFA) or microwave ablation (MWA), due to the more gentle effects on the kidney and collecting system and the visibility of the ablation zone, unlike other modalities. The risks to surrounding structures, such as bowel and the collecting system, are therefore less with cryoablation when compared to these technologies. 11
Along with the multidisciplinary team, the interventional radiologist can be consulted for small renal masses of less than 4cm located throughout the kidney, or even larger if necessary. With modern techniques most lesions can be treated safely and effectively. While most guidelines recommend that cryoablation treatments be reserved for elderly patients with comorbidities and an increased risk of complications after major surgery, the treatment can be considered as an option for patients of any age, especially if surgical treatments are contraindicated. By incorporating minimally invasive procedures such as cryoablation into RCC treatment pathways, healthcare professionals can ensure a more holistic, patient-centered approach to care, ultimately leading to improved outcomes and enhanced patient satisfaction.
Despite its multifactorial benefits, Western Australia was lacking a cryoablation service for RCC until recently. Having been in place successfully for several years now, the state’s successful cryoablation initiative illustrates the potential for broader national adoption. As interventional radiology specialists, we see ourselves as partners to urologists, oncologists and general practitioners, as we all have the same goal – to help our patients attain the best outcomes and care. Modern IR services, such as the WA service for RCC, extend beyond single procedures, offering initial consultation and follow-up, resulting in coordinated care that integrates with the patient’s broader treatment team.
Cryoablation for RCC is one example of how healthcare professionals can empower patients with knowledge and information on treatment options that may better suit their individual health needs. In doing so, we can play a critical role in facilitating informed discussions that can lead to optimal outcomes for both the patient and the healthcare system. By raising awareness and improving access to minimally invasive procedures, such as cryoablation for RCC, we can advance toward more holistic, patient-centered approaches in healthcare.
Cryoablation for RCC is a minimally invasive, safe, effective and cost-effective treatment, that is the only non-surgical treatment modality with long term data. Oncologists, urologists and GPs are encouraged to consult their local Interventional Radiologist about patients who may benefit from this procedure.
Dr Will Ormiston is a diagnostic and interventional radiologist at Sir Charles Gairdner and Hollywood Private Hospitals, Western Australia.
References
- Pierorazio PM, Johnson MH, Patel HD, Sozio SM, Sharma R, Iyoha E, et al. Management of Renal Masses and Localized Renal Cancer: Systematic Review and Meta-Analysis. J Urol. 2016 Oct;196(4):989–99.
- Australian Institute of Health and Welfare. (2023). Cancer data in Australia. Retrieved from https://www.aihw.gov.au/reports/cancer/cancer-data-in-australia.
- Ali S, Ahn T, Papa N, Perera M, Teloken P, Coughlin G, et al. Changing trends in surgical management of renal tumours from 2000 to 2016: a nationwide study of Medicare claims data. ANZ J Surg. 2020 Jan;90(1–2):48–52.
- Motzer RJ, Jonasch E, Agarwal N, Alva A, Baine M, Beckermann K, et al. Kidney Cancer, Version 3.2022, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2022 Jan;20(1):71–90.
- Morkos J, Porosnicu Rodriguez KA, Zhou A, Kolarich AR, Frangakis C, Rodriguez R, et al. Percutaneous Cryoablation for Stage 1 Renal Cell Carcinoma: Outcomes from a 10-year Prospective Study and Comparison with Matched Cohorts from the National Cancer Database. Radiology. 2020 Aug;296(2):452–9.
- Rivero JR, De La Cerda J, Wang H, Liss MA, Farrell AM, Rodriguez R, et al. Partial Nephrectomy versus Thermal Ablation for Clinical Stage T1 Renal Masses: Systematic Review and Meta-Analysis of More than 3,900 Patients. J Vasc Interv Radiol. 2018 Jan;29(1):18–29.
- Chan VWS, Abul A, Osman FH, Ng HHL, Wang K, Yuan Y, et al. Ablative therapies versus partial nephrectomy for small renal masses – A systematic review and meta-analysis. Int J Surg. 2022 Jan;97:106194.
- Finelli A, Ismaila N, Bro B, Durack J, Eggener S, Evans A, et al. Management of Small Renal Masses: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. 2017 Feb 20;35(6):668–80.
- Krokidis ME, Orsi F, Katsanos K, Helmberger T, Adam A. CIRSE Guidelines on Percutaneous Ablation of Small Renal Cell Carcinoma. Cardiovasc Intervent Radiol. 2017 Feb;40(2):177–91.
- Ljungberg B, Albiges L, Abu-Ghanem Y, Bedke J, Capitanio U, Dabestani S, et al. European Association of Urology Guidelines on Renal Cell Carcinoma: The 2022 Update. Eur Urol. 2022 Oct;82(4):399–410.
- Rosenberg MD, Kim CY, Tsivian M, Suberlak MN, Sopko DR, Polascik TJ, et al. Percutaneous Cryoablation of Renal Lesions With Radiographic Ice Ball Involvement of the Renal Sinus: Analysis of Hemorrhagic and Collecting System Complications. Am J Roentgenol. 2011 Apr;196(4):935–9.


